Fatigue and gait decline in adult cerebral palsyPhD dissertation by Anders Gravholt
Supervisors: Bruno Fernandes, Annemieke Buizer & Thomas Lapole,
Cerebral Palsy (CP) affects 1-3 children / 1000 births depending on the country investigated, with spastic diplegic forms being 35% of CPs. Due to an early brain injury occurring in the antenatal or postnatal phase, it causes alterations in motor function pertaining to posture and gait.
Commonly observed issues in CP include motor performance degradation during adulthood, with the underlying pathophysiology being unclear. One of the hypotheses to explain the decline in walking capacities in adults with CP is their greater fatigability, that could be related to energy overconsumption (due to the specific biomechanical constraints of their walking pattern) and/or the occurrence of early sarcopenia affecting the compensatory muscle mechanisms commonly seen in children to compensate for architectural disorders and posture alterations. Another hypothesis is that a decrease develops in motor control, leading to lower degrees of muscle activation, in turn leading to disuse atrophy.
Both of these hypotheses could explain an increased cost of locomotion, which in turn would lead to a decreased reserve capacity and premature fatigue. To optimize prevention and/or therapy in this population, it is crucial to better understand the aetiology of fatigability and its role in the decline in walking performance. Knowing this will allow us to prescribe interventions alleviating specific issues and possibly increase quality of life among adults with cerebral palsy. The primary objective of this project is thus to explore how fatigability and reduced walking performance are related. This will be possible thanks to an integrated approach (clinical, neuromuscular, biomechanical, and energetic).
Contract duration: 10/2022 to 10/2025
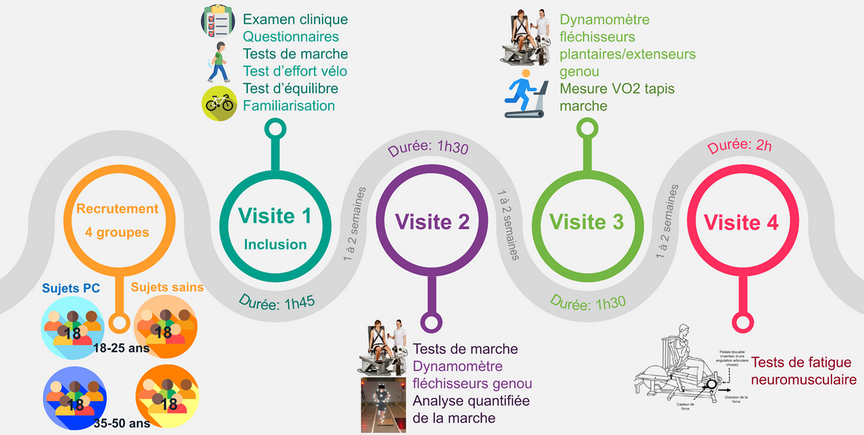
Subjects recruted from 2 ages groups with and without CP will undergo a series of visists one to two weeks apart for (1) inclusion checkup, and (2-4) repeated testing sessions.


 Université Jean Monnet
Université Jean Monnet